The immune system represents our primary line of defense against viruses and bacteria and plays a crucial role in eliminating tumor cells.

At the Department of Life Sciences of the University of Siena, Professor Francesca Finetti has focused her research on understanding how this complex system is activated and regulated.
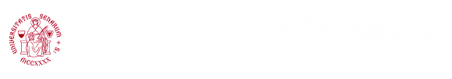
A central focus of her work is the immunological synapse, a highly specialized interface formed between two immune cells: a T lymphocyte and an antigen-presenting cell, which “displays the enemy” to be attacked. This structure is essential, as it enables the T cell to become activated, proliferate, and promote a targeted response against pathogens.
Leveraging her expertise in the immunological synapse, Professor Finetti is now investigating a specific disorder: Activated PI3Kδ Syndrome (APDS). In this rare genetic disease the PI3Kδ protein, a molecule essential for immune cell activation, is hyperactive even in the absence of stimuli, leading to an imbalance in immune responses. As a result, affected patients often present with recurrent infections, autoimmune disorders, and, in some cases, lymphatic cancers.
Despite recent advances, many aspects of APDS remain poorly understood. We asked Professor Finetti to tell us more about the IS-APDS research project, funded by the University of Siena under the 2024 New Frontiers program.
How did the idea for the IS-APDS project arise?
The project emerged from a collaboration with Professor Vassilios Lougaris, a medical researcher and Full Professor of Pediatrics at the University of GGG, and with Professor Cosima Baldari, Emeritus Professor at the Department of Life Sciences, University of Siena.
What is the main objective of the project?
Our goal is to investigate in detail the assembly of the immunological synapse in patients with APDS, in order to understand how genetic mutations affect this key structure. The project has two main aims: first, to elucidate the molecular mechanisms underlying the disease; and second, to identify potential biomarkers that may help predict symptom severity or assess the efficacy of available treatments. These insights are particularly important given that therapeutic options for APDS remain limited. Specific inhibitors, such as the drug leniolisib, are available, but it is not yet clear when and how they should be optimally used, nor what the long-term side effects might be.
Why is this research important?
Studying the immunological synapse in APDS patients allows us to understand what happens at the cellular and molecular levels in this disorder. It may also explain the wide variability of symptoms
among patients and, most importantly, pave the way for personalized therapies.
Although APDS is a rare disease, it offers a unique opportunity to explore the fundamental mechanisms of human immunity. A deeper understanding of how the immunological synapse functions – and what occurs when it fails – brings us closer to the goal of more precise, targeted, and personalized medicine, not only for APDS but also for other immune-related conditions.